Coronavirus: useful links
We are collecting information and links to useful local resources which we are updating regularly. […]
We are collecting information and links to useful local resources which we are updating regularly. […]
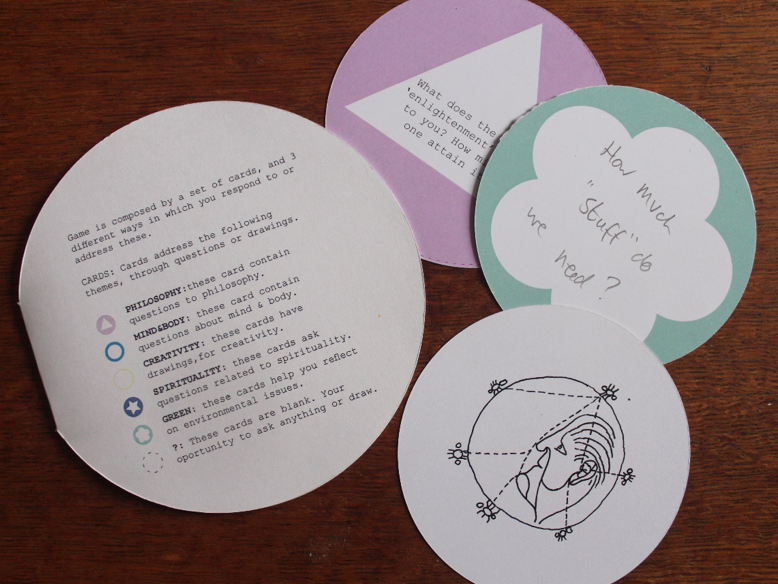
GAME: a board game co-designed by clients at the Psychosis Therapy Project Not every game […]

Outcome, Islington Mind’s client-led LGBTQ+ service, has been shortlisted for Charity or Non-Profit Organisation of […]